Osteoarthritis of the hip joint is a degenerative-dystrophic pathology, characterized by the destruction of the hyaline cartilage.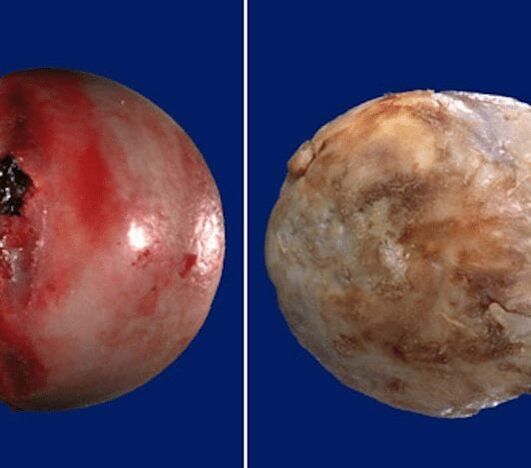 The disease develops gradually, accompanied by pain and decreased range of motion. In the absence of medical intervention in the initial stage of osteoarthritis, after a few years, atrophy of the femoral muscles occurs.
The disease develops gradually, accompanied by pain and decreased range of motion. In the absence of medical intervention in the initial stage of osteoarthritis, after a few years, atrophy of the femoral muscles occurs. The injured limb is shortened and joint space fusion leads to partial or complete immobilization of the hip joint. The causes of pathology are previous injuries, curvature of the spine, systemic diseases of the musculoskeletal system.
The injured limb is shortened and joint space fusion leads to partial or complete immobilization of the hip joint. The causes of pathology are previous injuries, curvature of the spine, systemic diseases of the musculoskeletal system.
Osteoarthritis is usually found in middle-aged and elderly patients. Diagnosis is made on the basis of the results of instrumental studies: radiography, MRI, computed tomography, arthroscopy. The treatment of pathology of 1 and 2 degrees of severity is conservative. If ankylosis is detected or drug therapy is ineffective, a surgical operation (arthrodesis, endoprosthesis) is performed.
The mechanism of development of pathology.
The hip joint is made up of two bones: the ilium and the femur. The lower part of the ilium is represented by your body, which participates in the articulation with the femur, forming the upper part of the acetabulum. During movement, the glenoid fossa is immobile and the femoral head moves freely. Such a device of "hinge" of the hip joint allows you to bend, bend, rotate, promote abduction, adduction of the hip. The soft, strong and tough hyaline cartilage that lines the acetabulum and the femoral head provides unhindered gliding of joint structures. Its main functions are the redistribution of loads during movement, prevention of rapid wear of bone tissues.
Under the influence of external or internal factors, cartilage trophism is disturbed. It does not have its own circulatory system: the synovial fluid supplies nutrients to the tissue. With osteoarthritis, it thickens, becomes viscous.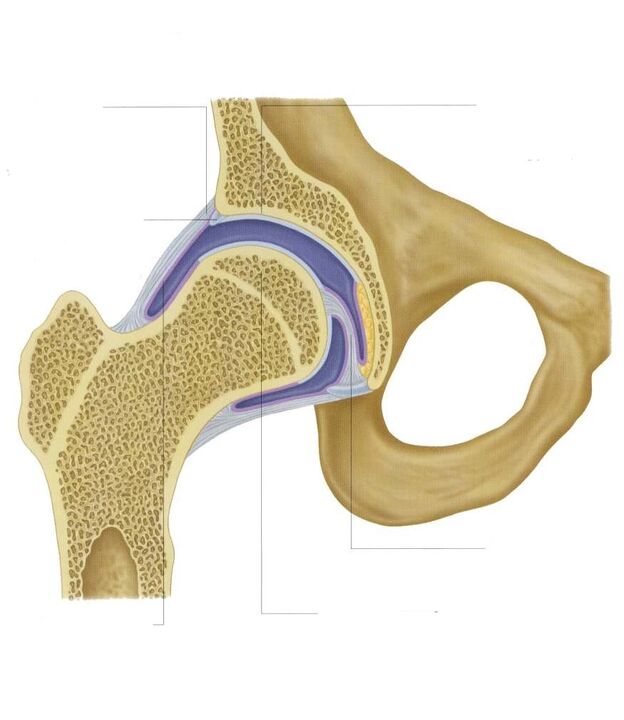 The resulting nutrient deficiency causes the hyaline cartilage surface to dry out. It becomes covered with cracks, which leads to permanent microtrauma to the tissues during flexion or extension of the hip joint. Cartilage thins and loses its shock-absorbing properties. The bones deform to "adapt" to the increased pressure. And against the background of deterioration of metabolism in tissues, destructive and degenerative changes progress.
The resulting nutrient deficiency causes the hyaline cartilage surface to dry out. It becomes covered with cracks, which leads to permanent microtrauma to the tissues during flexion or extension of the hip joint. Cartilage thins and loses its shock-absorbing properties. The bones deform to "adapt" to the increased pressure. And against the background of deterioration of metabolism in tissues, destructive and degenerative changes progress.
Causes and provoking factors.
Idiopathic or primary osteoarthritis develops for no reason. It is believed that the destruction of cartilage tissue occurs due to the natural aging of the body, slowing down of recovery processes, decreased production of collagen and other compounds necessary for the full regeneration of the structures of the hip joint. Secondary osteoarthritis occurs against the background of a pathological condition already present in the body. The most common causes of secondary disease include:
- previous injuries: damage to the ligamentous tendon apparatus, muscle tears, its complete separation from the bone base, fractures, dislocations;
- violation of joint development, congenital dysplastic disorders;
- autoimmune pathologies: rheumatoid, reactive, psoriatic arthritis, systemic lupus erythematosus;
- nonspecific inflammatory diseases such as purulent arthritis;
- specific infections: gonorrhea, syphilis, brucellosis, ureaplasmosis, trichomoniasis, tuberculosis, osteomyelitis, encephalitis;
- disruption of the functioning of the endocrine system;
- degenerative-dystrophic pathologies: osteochondropathy of the femoral head, dissecting osteochondritis;
- hypermobility of the joints, due to the production of "super-extensible" collagen, causing their excessive mobility, weakness of the ligaments.
Since the cause of the development of osteoarthritis can be hemarthrosis (bleeding in the cavity of the hip joint), provoking factors include disorders of hematopoiesis. The prerequisites for the onset of the disease are excess weight, excessive physical activity and a sedentary lifestyle. Its development is caused by improper organization of sports training, a deficiency in the diet of foods with a high content of microelements, water-soluble vitamins and fats. Postoperative osteoarthritis occurs several years after surgery, especially if it was accompanied by the excision of a large amount of tissue. Hyaline cartilage trophism is disturbed by frequent hypothermia, living in an environmentally unfavorable environment, and working with toxic substances.
Osteoarthritis of the hip joint cannot be inherited. But in the presence of certain congenital features (metabolic disorders, skeletal structure), the probability of their development increases significantly.
Symptoms
The main symptoms of osteoarthritis of the hip joint are pain when walking in the hip region, radiating to the groin and knee joint. A person suffers from stiffness of movements, stiffness, especially in the morning. To stabilize the joint, the patient begins to limp, his gait changes. Over time, due to muscle atrophy and joint deformation, the limb is noticeably shortened. Another characteristic sign of the pathology is the limitation of hip abduction. For example, difficulties arise when trying to sit on a stool with legs spread apart.

For osteoarthritis of the first severity, periodic pain occurs after intense physical exertion. They are located in the joint area and disappear after a long rest.
With osteoarthritis of the second degree of the hip joint, the severity of the pain syndrome increases. Discomfort occurs even at rest, spreads to the thigh and groin, increases with lifting weights or with increased motor activity. To eliminate pain in the hip joint, a person begins to limp just noticeably. Limitation of movement in the joint is noted, especially during abduction and internal rotation of the thigh.
Third degree osteoarthritis is characterized by intense and constant pain that does not subside during the day and night. Difficulties arise when moving, therefore, when walking, a person is forced to use a cane or crutches. The hip joint is stiff, there is a significant atrophy of the muscles of the buttocks, thighs and legs. Due to the weakness of the abductor femoral muscles, the pelvic bones are displaced in the frontal plane. To compensate for the shortening of the leg, the patient leans toward the injured limb when moving. This causes a sharp shift in the center of gravity and increased stress on the joint. At this stage of osteoarthritis, a pronounced ankylosis of the joint develops.
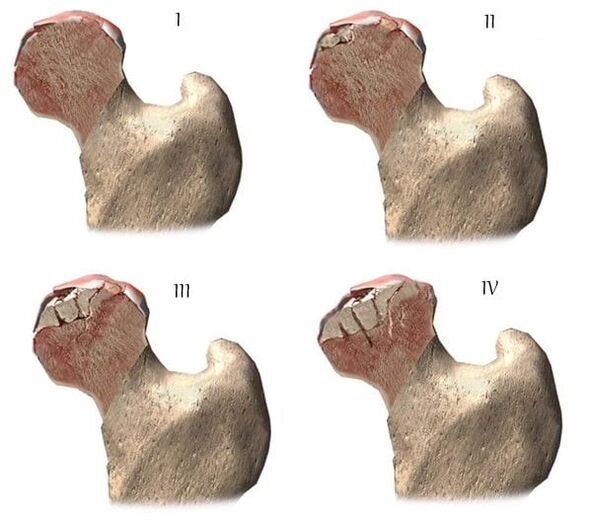
| Degrees | Radiographic signs |
| First | The changes are not pronounced. Joint spaces are moderately and unevenly reduced, there is no destruction of the surface of the femur. Minor bony growths are seen on the outer or inner border of the acetabulum. |
| The second | The height of the joint space is significantly reduced due to its uneven fusion. The bony head of the femur is displaced upward, deformed, enlarged, and its contours become uneven. Bony growths form on the surface of the inner and outer edges of the glenoid fossa |
| Third | There is a complete or partial fusion of the joint space. The femoral head is strongly expanded. Multiple bony growths are found on all surfaces of the acetabulum. |
Diagnostics
When making a diagnosis, the doctor takes into account the clinical manifestations of the pathology, the anamnesis, the results of an external examination of the patient, and instrumental studies. Radiography is the most informative. With the help of him, the state of the hip joint, the stage of its course, the degree of damage to cartilaginous tissues is assessed, and in some cases the cause of development is established. If the cervico-diphysial node is enlarged and the acetabulum is oblique and flattened, then with a high degree of probability it is possible to assume dysplastic congenital changes in the joint. Perthes disease or juvenile epiphysiolysis is indicated by the altered shape of the hip bone. Radiography may reveal post-traumatic osteoarthritis, despite the absence of previous trauma in the history. Other diagnostic methods are also used:
- CT helps to detect the growth of the edges of the bone plates, formed osteophytes;
- Magnetic resonance imaging is performed to assess the state of connective tissue structures and the degree of involvement in the pathological process.
If necessary, the inner surface of the joint is examined with arthroscopic instruments. Differential diagnosis is made to exclude gonarthrosis, lumbosacral or thoracic osteochondrosis. Pain in osteoarthritis can be disguised as clinical manifestations of radicular syndrome caused by entrapment or inflammation of the nerves. Usually it is possible to exclude neurogenic pathology with the help of a series of tests. Osteoarthritis of the hip joint is necessarily differentiated from trochanteric bursitis of the hip joint, ankylosing spondylitis, and reactive arthritis. To exclude autoimmune pathologies, biochemical studies of blood and synovial fluid are performed.
Drug treatment tactics
Medical treatment is aimed at improving the well-being of the patient. For this, drugs of various clinical and pharmacological groups are used:
- Non-steroidal anti-inflammatory drugs (NSAIDs): nimesulide, ketoprofen, diclofenac, ibuprofen, meloxicam, indomethacin, ketolac. Injectable solutions are used to relieve acute pain, and pills, pills, ointments, and gels help to eliminate pain of mild or moderate intensity;
- glucocorticosteroids: triamcinolone, dexamethasone, hydrocortisone. They are used in the form of intra-articular blocks in combination with anesthetics Procaine, Lidocaine;
- muscle relaxants: baclofen, tizanidine. Included in treatment regimens for skeletal muscle spasms, pinching of sensitive nerve endings;
- drugs that improve blood circulation in the joint: nicotinic acid, aminophylline, pentoxifylline. They are prescribed to patients to improve tissue trophism, prevent disease progression;
- chondroprotectors. Effective only in stages 1 and 2 of osteoarthritis.
Rubbing warming ointments helps to remove mild pain. The active ingredients of external agents are capsaicin, cinquefoil, camphor, menthol. These substances are characterized by an irritating and distracting local analgesic effect. Compress the joints with dimethyl sulfoxide, medical bile will help to cope with swelling, morning thigh swelling. Classic, acupressure or vacuum massage for coxarthrosis is recommended for patients. Daily exercise therapy is an excellent prevention of further progression of osteoarthritis.
Surgical intervention
With the ineffectiveness of conservative therapy or the diagnosis of a pathology complicated by ankylosis, an operation is performed. It is impossible to restore cartilage tissue in the joint damaged by arthrosis without prosthetic surgery, but with the correct approach to treatment, compliance with all medical prescriptions, maintaining a correct lifestyle, conducting therapeutic exercises, courses ofregular massage, taking vitamins and proper nutrition. , can stop the process of injury and destruction of cartilage and hip joints.






















